Nothing puts a damper on your day faster than a throbbing headache. Headaches affect almost 50% of the population every year. And they originate from many sources. There are over 150 types of headaches!

This article covers the most common types of headache and the best treatments for each. And you’ll learn how exercises and physical therapy can provide relief.
Tension Headaches
Also known as stress headaches, tension type headaches account for up to 80% of all headaches.
What causes tension headaches?
Muscle tightness in the neck, jaw and head muscles causes tension headaches. Triggers include poor sleep, anxiety, high stress levels, eye strain, fatigue, and poor sitting posture (1).
Also, tension headaches originate from sleeping wrong on your neck, working on computer, or playing too much Wordle and Candy Crush on your phone.
Females experience tension headaches more often than males. And genetic factors influence tension headaches.
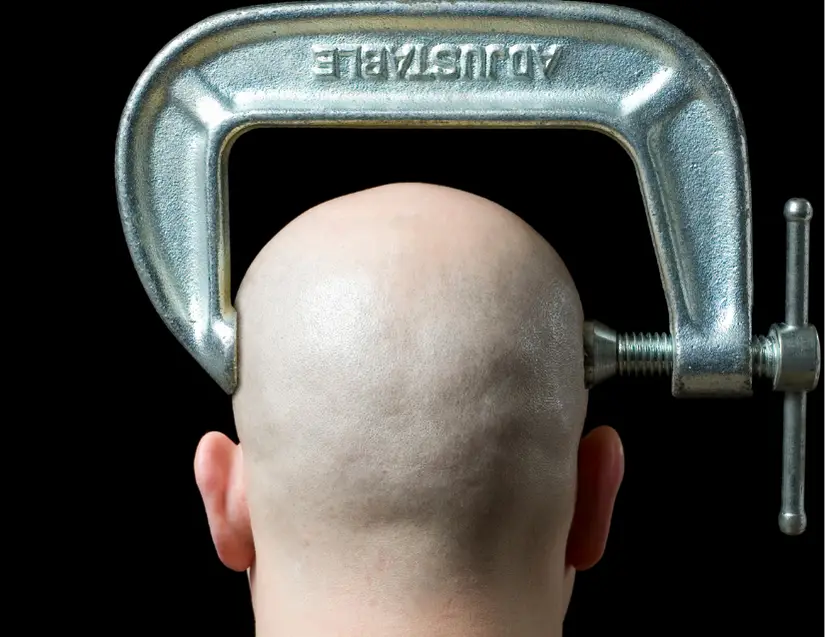
Tension headaches feel like a vice is squeezing your head. Pain occurs in the forehead, sides, and top of the head. Headaches are bilateral, affecting both sides of your head.
What are the best treatments for tension headaches?
There are many effective treatments for tension type headaches.
1. Stress Management

Research shows a close link between stress and pain. Managing stress is key for tension headache relief. Try deep breathing, yoga or meditation. Even a walk through nature will relieve stress.
Cognitive behavioral therapy (CBT) is another proven stress relief strategy. CBT often works better than medication for conditions like depression, anxiety, insomnia and even low back pain (2).
2. Massage

Soft tissue treatment reduces neck and headache sensitivity. Getting a massage or using percussion therapy can unlock tight spots in your muscles.
3. Posture

Practice good posture when sitting, reading, working on the computer and using your phone. To learn how, check out this article: 5 Ways to Sit With Less Pain
4. Medication

Ask your doctor or pharmacist about this one. Over-the-counter pain medications and muscle relaxers can ease tension headaches.
5. Dry Needling

Trigger point dry needling relieves muscle tightness. It’s a proven treatment to reduce pain and disability from tension headaches (3).
Neck Pain with Headaches (Cervicogenic)
Cervicogenic headaches are closely related to tension headaches. Cervicogenic headaches start in the neck and affect one side of the head (4).
What causes cervicogenic headaches?
Cervicogenic headaches emanate from the upper cervical spine, C1 through C3. As their name suggests, neck pain is a key feature of this type of headache. Joint and muscle tightness contribute to cervicogenic headaches.

The upper cervical spine is responsible for neck rotation (turning right and left like an owl). So stiffness with neck rotation is a common component of cervicogenic headaches. Limited rotation motion is typically worse towards the painful side.
Cervicogenic headaches worsen with prolonged neck positioning in awkward positions. Aggressive neck motion also exacerbates them. Cervicogenic headaches usually last a few minutes to a few hours.
What treatments are best for cervicogenic headaches?
Physical therapy is your best bet for neck pain with headaches. Current guidelines (5) recommend these treatments:
1. Neck Mobility Exercises
The best cervicogenic headache exercises restore neck rotation. This exercise, a sustained natural apophyseal glide (SNAG) targets neck rotation in the upper cervical spine, between C1 and C2.
Physical therapists use this drill to regain neck rotation towards the painful, stiff side.
2. Manual Therapy
Manual therapy is professional hands-on treatment to reduce joint and muscle stiffness. For cervicogenic headaches, your PT will use manual therapy on and around your upper cervical spine.

Mobilizing joints and muscles in surrounding regions (like the neck and thoracic spine) can help, too.
3. Neck Manipulation
Having your neck cracked or popped doesn’t realign bones that are out of position (6). This treatment primarily affects the nervous system and does improve joint motion and reduce pain.
Some physical therapists (like me) opt not to manipulate the cervical spine because of rare but serious side effects. However, neck manipulation is considered safe enough to be included in physical therapy treatment guidelines (5).
Learn more about spinal manipulation from this NIH article: Spinal Manipulation: What You Need To Know
4. Postural Strength
Strong neck and upper back muscles reduce strain on the neck. Strength breeds durability.

Try lawnmower rows (above) to strengthen your trapezius, rhomboid and latissimus dorsi muscles.
5. Neck Strength
Neck strengthening exercises reduce neck pain (7).
This exercise may look easy, but it’s a tough exercise that strengthens the front of the neck.
Migraine Headaches
Migraines cause moderate to severe headaches. Most migraines are unilateral (one-sided) and come with light or sound sensitivity.

Migraines are genetic and plague women 3x more than men; they afflict 17% of females and 6% of males.
What causes migraines?
Experts used to believe that blood flow changes in the brain cause migraines. But that theory is outdated (8).
Now, scientists believe that migraines result from a complex series of chemical events in the brain. To learn more, you can read all about the glial depolarization and pannexin-1 megachannel opening here.
Many factors contribute to migraines. Common triggers include stress, hormone changes, skipping meals, weather changes and lack of sleep.
Studies show more trigger points (muscle knots) in neck muscles of people who experience migraines than those who don’t. These trigger points increase the body’s sensitivity to pain and exacerbate headaches (9).
What treatments work for migraines?
1. Trigger Point Treatments
Treatments like dry needling, manual therapy, and percussion therapy seem to reduce migraine attacks, though more research is warranted (10).
2. Medication
This is the most common approach to treating migraines. Finding the right medication (or drug combination) often takes time and expertise.

So it’s vital to work with a skilled medical doctor or pharmacist to manage migraine headaches.
3. Lifestyle Changes
These include regular exercise, relaxation training, yoga, reducing triggers and cognitive behavioral therapy. CBT is a powerful tool to reduce tension and migraine headaches, according to the American Headache Society.
Red Flags
Most headaches are innocuous. In fact, nearly half of all adults experience at least one headache in a year (11).

But in rare cases, headaches indicate a serious medical problem. These “red flag” signs warrant medical attention:
- Nausea
- Vomiting
- Bilateral arm symptoms
- Fainting
- Trouble speaking or swallowing
- Vision changes
- Dizziness
- Thunderclap headaches
- Progressive headache worsening for weeks
When in doubt, talk with a qualified healthcare provider.
Wrapping Up
In summary, most headaches are tension headaches. Tension headaches and cervicogenic headaches respond positively to lifestyle changes and physical therapy. Even migraines may benefit from physical therapy interventions.
If you are experiencing headaches, consult with a medical doctor or physical therapist to gain control of your pain.
For more practical tips to manage pain and improve your health, join the free, fast-growing Facts & Physio Newsletter. Plus, get The Recovery Checklist when you sign up.

