Back pain affects 80% of us at one time or another (1). Science has enhanced our understanding of low back pain. We’ve discarded worthless treatments over the years.
Centuries ago, people thought low back pain came from a being shot by a witch. Treatment involved burning the patient with flaming goat dung. Or using special powers in babies’ feet to treat the sore back (2). Thankfully, treatments have evolved. (And no, none of these methods work. Don’t try them at home.)
Research still tells us which treatments do and don’t work. But back pain treatment isn’t always consistent with scientific evidence.
Here are 5 common, harmful mistakes; avoid these to boost your odds of successful recovery.
This is what not to do.
1) Panic
Panic is a normal response to back pain. Especially if the pain is new or severe. Here’s the good news: 99.1% of low back pain isn’t a serious medical problem (3).

Don’t let your imagination run amok. Fearing the worst, known as “catastrophization,” is associated with worse outcomes for people with low back pain (4). And fear frequently contributes to chronic pain (5).
Fear stops us in our tracks. When we’re fearful, we move less and enjoy fewer of our normal day-to-day activities. This can prolong recovery. In contrast, light movement (even through discomfort) restores confidence, provides nutrition to the spine and puts us on track for a successful recovery.
This quote captures it perfectly:
“The only thing to fear is fear itself…when it comes to low back pain” -FDR (probably)
If fear is hindering your recovery, you may benefit from cognitive behavioral therapy.
Rooted in the Greek philosophy of Stoicism, cognitive behavioral therapy often works better than medication for treating insomnia, anxiety, and chronic low back pain (6).
2) Get Unneeded Imaging
Often, getting an X-Ray or MRI isn’t beneficial. Here are 4 reasons why guidelines recommend against imaging for most cases of low back pain:
a) Cost
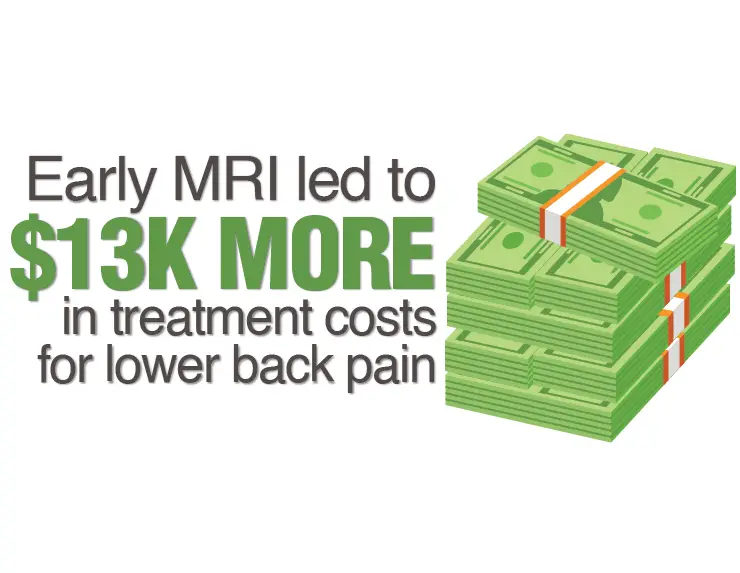
MRIs are expensive. And that’s just the beginning. Treatment costs can climb quickly after an MRI.
One low back pain study (7) compared patients who got an early MRI (within 30 days of onset) to those who didn’t. The early MRI group paid $13,000 more in total treatment costs than the group who didn’t get the early MRI. $13,000! That could fund a few fun weeks of retail therapy.
b) Outcomes
Here’s the craziest part of the MRI study: For $13,000 more, the early MRI group must have gotten better results, right?
Nope.
Their outcomes were worse(!!), even after researchers controlled for demographics and low back pain severity. The early MRI group was more disabled and more likely to have spine surgery.
c) Correlation to Symptoms
MRI and X-Ray findings correlate poorly with symptoms, especially in acute low back pain (7,8,9). Findings like disk bulges, arthritis and disk degeneration are normal in people without back pain (10).
For example, 52% of healthy, pain-free 30-year-olds have lumbar disk degeneration (10). Since these findings appear in healthy people, it’s difficult to know when they’re relevant to someone with back pain.

Hence why I’ve argued that bulging disks are no big deal.
d) Effect
Some chiropractors use spine X-Rays in routine clinical practice. But a recent systematic review by a chiropractic journal found that “Strong evidence demonstrates risks of imaging such as excessive radiation exposure, overdiagnosis, subsequent low-value investigation and treatment procedures, and increased costs.” (11). The study concluded “The use of spinal X-rays should not be routinely performed in chiropractic practice.”
This conclusion is consistent with imaging recommendations from Ghana, Europe, and the United States (12). Unneeded imaging rarely changes treatment. When it does, it’s often for the worse.

In PT school, it was drilled into my head: “treat the patient, not the image.” A patient’s symptoms and movement limitations matter more than a picture of their spine.
Taking a picture of your car’s engine won’t tell you why it’s making a strange noise. Often, lumbar imaging is just as useful.
Don’t get me wrong. There are times when imaging is absolutely recommended and necessary (8).
Lumbar imaging helps rule out serious medical pathology when patients display “red flag” symptoms. It’s warranted with severe, progressive neurologic deficits (muscle atrophy, progressive leg weakness). And it can be useful for cases with radicular symptoms (nerve pain in the leg) if 6 weeks of conservative treatment is unsuccessful (8).
Please consult with a qualified healthcare provider if you have questions about whether your symptoms warrant imaging. I’m relaying current guidelines and research, not making a recommendation one way or the other.
If you have nerve pain (sciatica) from your lower back, check out these proven exercises to relieve pinched nerve pain.
3) Bed Rest
Should you stay in bed for a few days to let those damaged tissues heal?

Nope.
This used to be a standard recommendation after back injury. It’s actually a bad idea.
Resting in bed is less effective than staying active (13). Plus, muscles atrophy with prolonged bed rest. Muscle strength plummets 40% after just 1 week of immobilization (14). Don’t lose those hard-earned muscles by staying in bed!
Guidelines recommend resuming work and normal daily activities, even if they are painful (15).
Ignoring pain isn’t a great idea (more on this in #4). But laying in bed panicking about back pain is a recipe for a long recovery.
Early physical therapy treatment accelerates the recovery process (15).
Patients who went to physical therapy within 4 weeks of pain onset had fewer back injections and fewer physician visits than those who went to PT >3 months after symptoms began. Plus, patients receiving early treatment developed chronic symptoms just 2% of the time. The delayed treatment group had chronic symptoms in 15% of cases (15).
Want to learn 3 simple, effective stretches to alleviate low back pain? Check out 3 Powerful Exercises to Reduce Low Back Pain
4) Ignore Pain
Bed rest is one extreme. Ignoring pain is the other.

It’s heroic, bold, admirable to battle through extreme pain. It’s Jordan with the flu, dominating Game 6 in 1997. It’s Tiger winning the 2008 U.S. Open on a broken leg.
For those of us who aren’t Jordan or Tiger, it’s a bad idea. Pain is our body’s alarm system. It alerts us when something is wrong.
People who can’t feel their feet have much higher risks of foot injury, sores and damage. Pain protects our body and helps us survive. Modifying painful activities alleviates irritation and creates an environment for healing.
5) Rely on Passive Treatments
Passive treatments are done to you, instead of by you.

Sure, there’s a place for passive treatments. Research supports spinal manipulation and dry needling for back pain (16,17,18). Other passive treatments can help control pain. This includes ice, heat, electrical stimulation and using a back brace.
But focusing solely on passive treatments is sub-optimal. Patients recover faster when they take an active role in managing their pain. Early, active treatments help the most with low back pain (15). And the best physical therapists involve and empower their patients during the rehab process (19).
Passive treatments may help the recovery process. But they shouldn’t define it.
Treat Your Own Back is a best-selling book that has helped thousands of people take control of their back pain (myself included) with an active approach.
Summary
The science is clear–avoid these common mistakes and you’ll recover faster.
Panic is counterproductive. So is unnecessary imaging. Bed rest produces worse outcomes than an active approach. Ignoring pain isn’t a great strategy. And active treatments work better than passive treatments.
I made most of these mistakes when I hurt my low back as a teenager. I failed rehab multiple times. Learning more and applying the strategies in Treat Your Own Back made all the difference for me.
Want to recover faster? Join the free Facts & Physio Newsletter and get The Recovery Checklist when you sign up.
References
- https://www.ncbi.nlm.nih.gov
- https://www.tandfonline.com
- https://pubmed.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://pubmed.ncbi.nlm.nih.gov
- https://ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://chiromt.biomedcentral.com
- https://www.ncbi.nlm.nih.gov
- https://www.cochranelibrary.com
- https://extremephysiolmed.com
- https://www.jospt.org
- https://www.sciencedirect.com
- https://www.ncbi.nlm.nih.gov
- https://www.bmj.com
- https://academic.oup.com


1 thought on “5 Low Back Pain Mistakes Proven to Prolong Recovery”
I have pain all the way from hip on my right side down.
It’s puzzling me still since Day one that this pain all started or is coming from my Back?
I am in Terrible Pain . as not sure if Physical Therapy wouldn ‘t harm me , I worry It would worsen this pain I’m having
and even injure me ., but after reading here. I hope to have made the right decision. I will try going to Physical Therapy
only time can truly get the answer. For, I feel this pain right now . itsn’t solvable .