Bulging discs, degenerative disc disease, disc herniations, bone spurs. These scary findings show up on many X-Rays and MRIs, worrying patients.
By the end of this article you will understand why these issues aren’t as worrisome as they sound.
Spine Anatomy
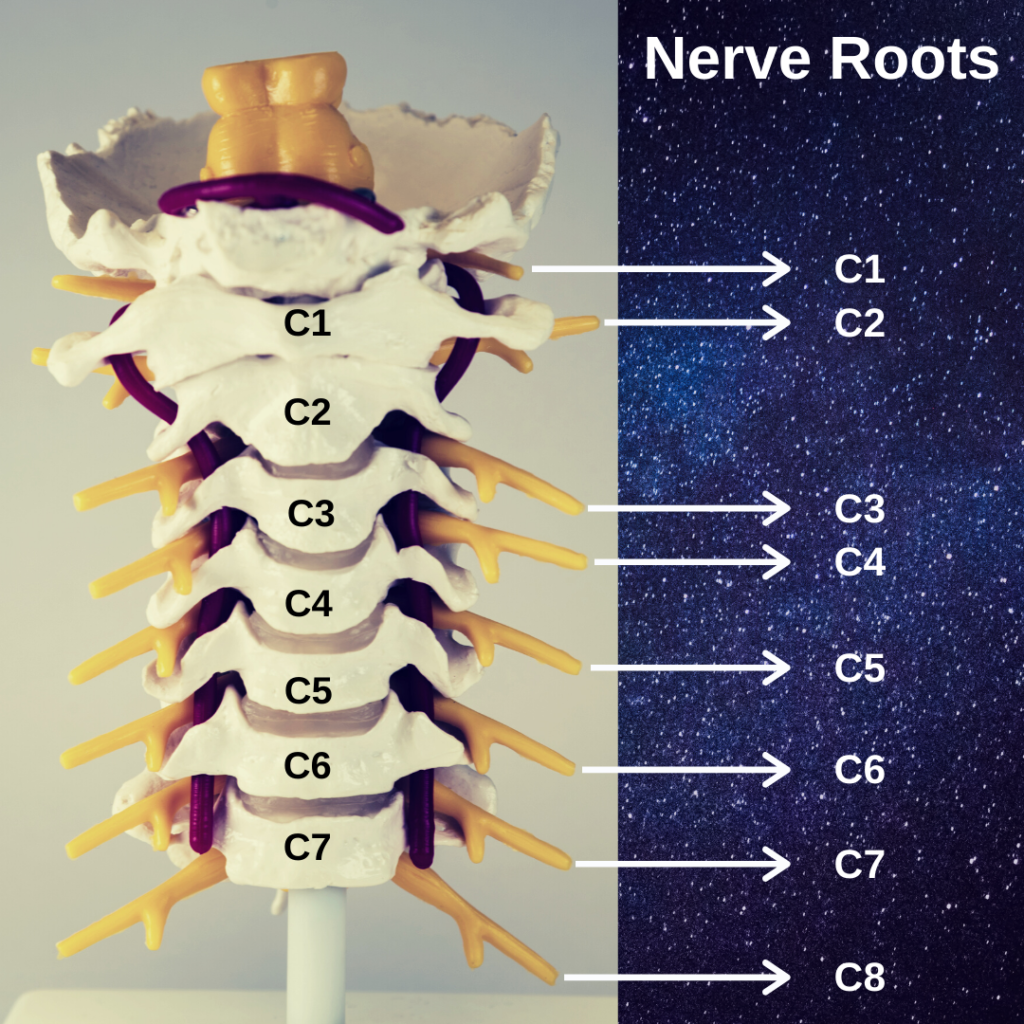
The spine encloses and protects the spinal cord. Nerves exit the spine and supply strength and sensation to the body.
Nerve irritation usually occurs at the nerve root where the nerve exits the spine. Also called a pinched nerve, this issue causes electricity-like pain in the arm, torso or leg, depending on which nerve root is irritated.
Nerve irritation in the neck, called cervical radiculopathy, cause pain in the shoulder, arm, and hand. Thoracic nerve irritation creates mid back and ribcage pain. A pinched nerve in the lower back causes hip, leg and foot symptoms–colloquially known as sciatica.
This graphic illustrates the nerve roots in the cervical spine (neck).
As their name suggests, intervertebral discs sit between the vertebrae (spine bones). Discs often get blamed for low back pain and neck pain, but they play a crucial role in the spine’s function.
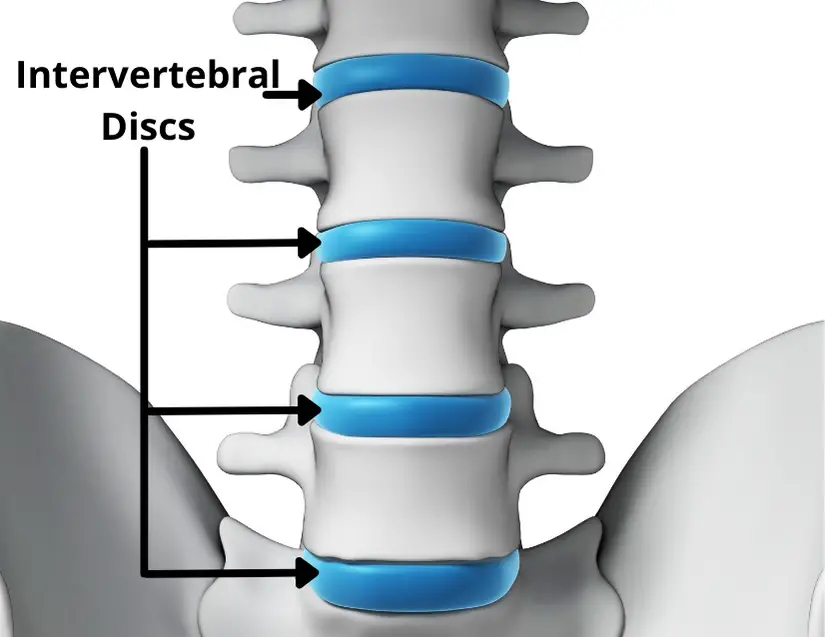
Intervertebral discs act like shocks, absorbing force and cushioning the spine. Discs have a thick, cartilaginous outer region called the annulus fibrosis. Inside the annulus fibrosis sits the gel-like nucleus pulposus (NP).
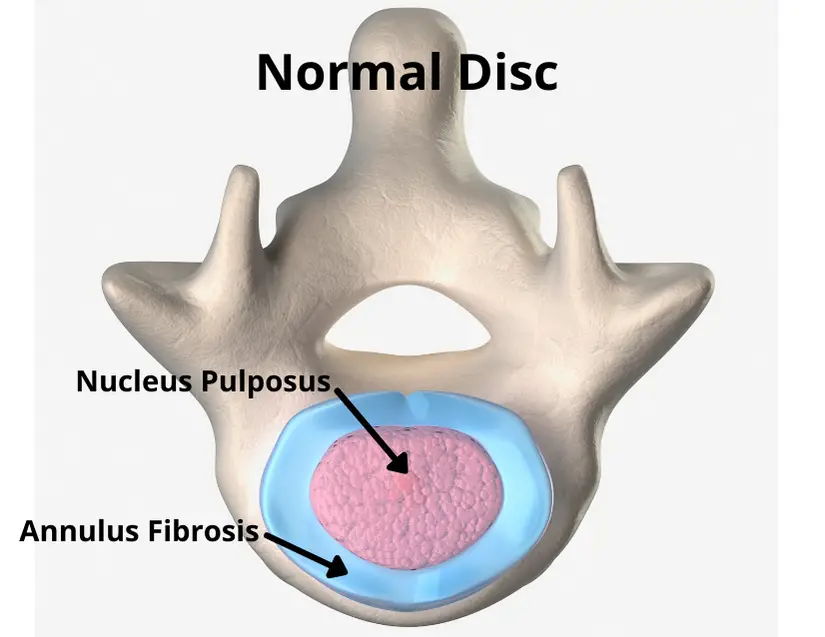
Here’s a bird’s eye view:
Terms to Know
So what does it mean to have a bulging disc? Or degenerative disc disease?
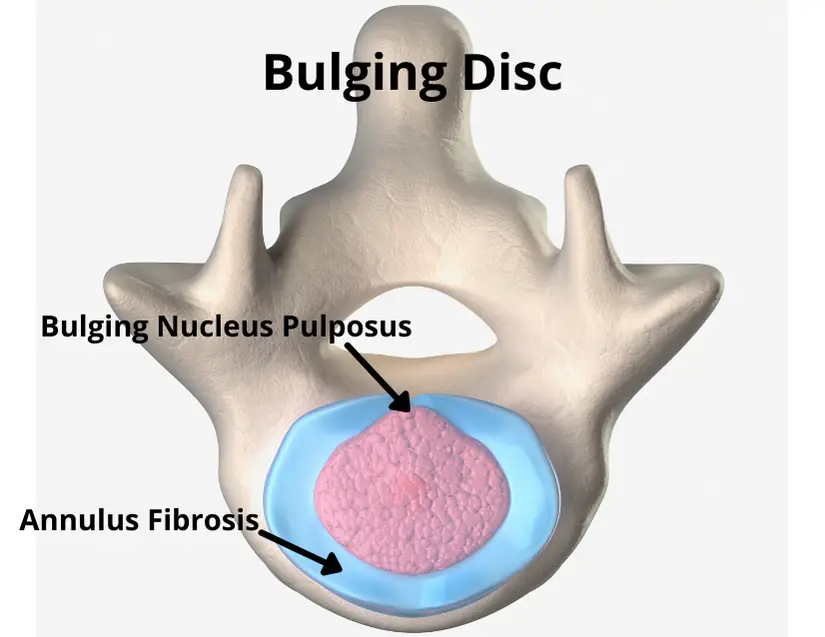
Anatomically, here’s what it looks like:
Bulging Disc
The nucleus pulposus–the gel-like inside of the disc–pushes on the annulus fibrosis and enlarges its footprint.
Herniated Disc
The inner disc material pushes through the annulus fibrosis–it’s more displaced than a bulging disc.
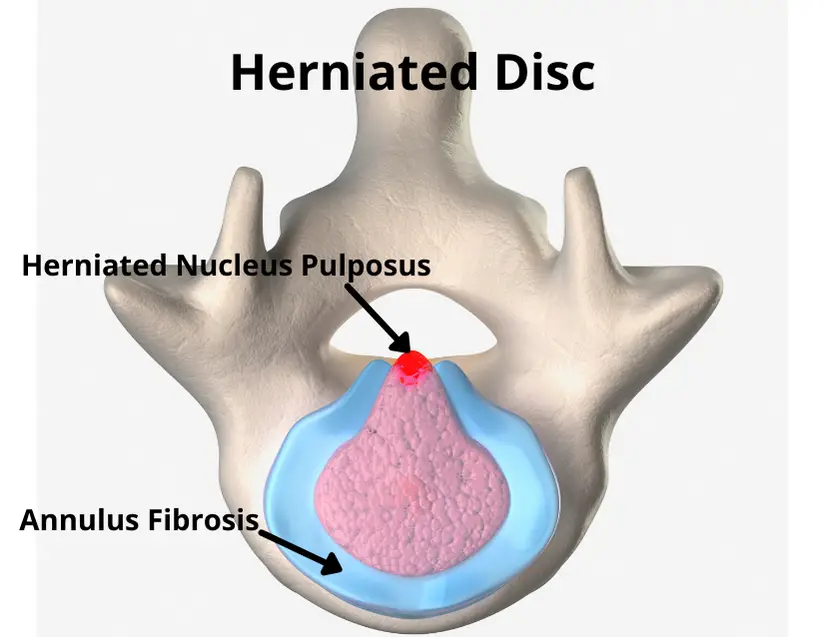
Even massive disc herniations respond well to conservative treatment, and 90% of herniated discs feel better within 6 months (1).
Extruded Disc
An extruded disc means a portion of the nucleus pulposus is outside the annulus fibrosis. Anatomically this is the most severe disc issue, but it also heals the fastest (2).
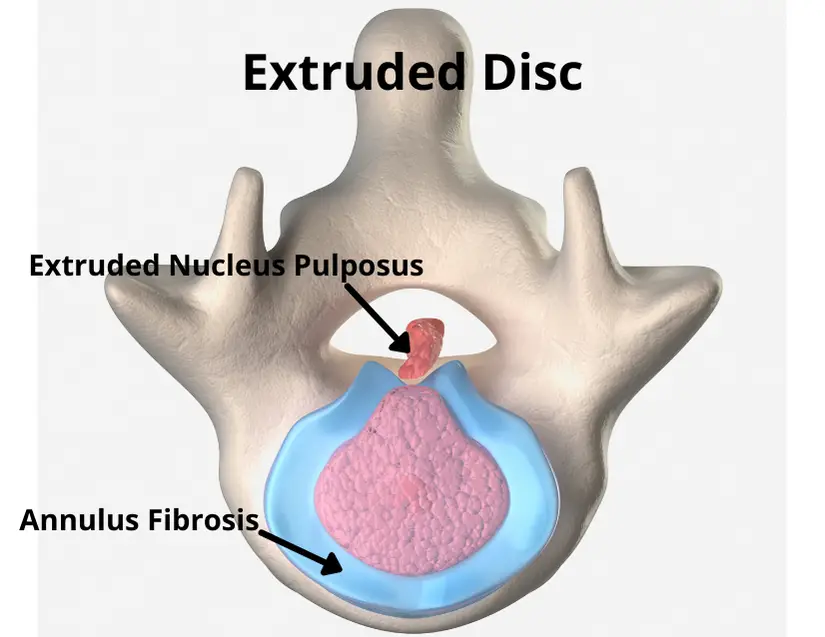
Most disc bulges/herniations/extrusions occur posteriorly, as depicted above. Fortunately, the posterior longitudinal ligament (not shown) prevents many disc bulges from pressing on the spinal cord, which sits behind the disc.
Degenerative Disc Disease
DDD sounds pretty scary. But it’s actually quite common. It simply means the disc has lost height.
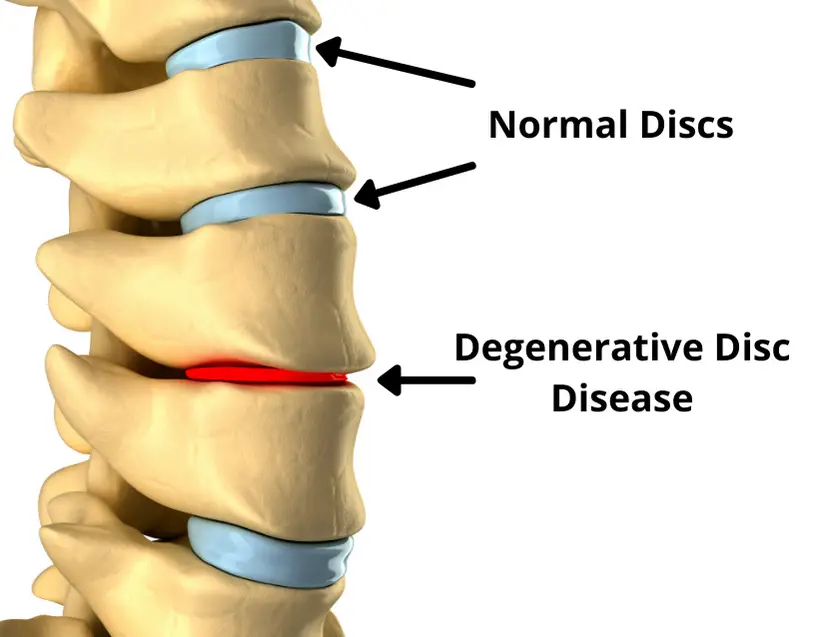
It’s a normal imaging finding, even for people without spine pain. Keep reading to find out just how prevelant DDD is in the pain-free population.
Bone Spurs
Bone spurs, also called osteophytes, are small areas of extra bone growth. They rarely cause pain and show up frequently on imaging.
Bone spurs and DDD are synonymous with spine arthritis. Extensive literature shows that arthritis is a normal part of the aging process and often uncorrelated to pain. Most people with spine arthritis do not have pain (3).
When Getting an MRI is Harmful
Getting an MRI for low back pain is often harmful. Early MRI leads to higher treatment costs, worse outcomes, and higher likelihood of surgery (4).
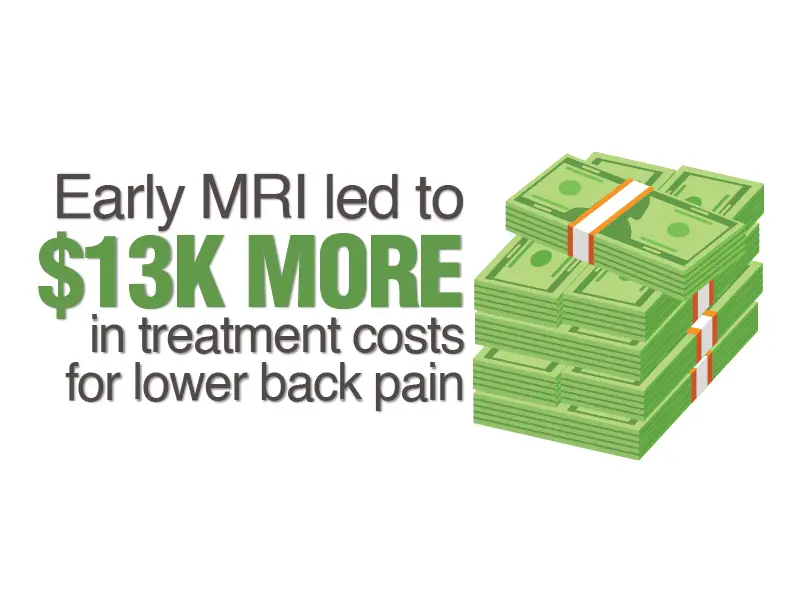
MRI findings typically sound bad, like the spine is damaged. This causes negative beliefs like “I shouldn’t move” or “my spine is fragile.” Negative beliefs and low expectations delay recovery and increased likelihood of chronic pain (5).
For more on why getting MRI is usually a bad idea for back pain, check out 5 Low Back Pain Mistakes Proven to Prolong Recovery.
Bulging Discs are Normal
If you randomly picked 100 middle-aged people off the street, ages 40 to 60, guess how many would have bulging discs.
5? 10? Maybe even 20?! Research says it’s 60!
60% of healthy, pain-free middle aged adults have bulging discs (6).
Therefore, it’s no surprise bulging discs are poorly correlated to pain (7). It’s the same with bone spurs, DDD, and other MRI findings. They’re common in pain-free individuals and usually don’t correlate well to pain.
Most notably, degenerative disc disease is clearly a normal part of aging. By age 80, 96% of pain-free individuals have DDD in their spine (6).
Arthritic changes in the spine are like getting facial wrinkles as we get older. It’s bound to happen, and it typically doesn’t cause any problems.
Is Imaging Useless?
No, X-Rays and MRIs can play an important role for spine pain. Imaging is the best tool for ruling out rare conditions like fractures, tumors and spinal cord compression.

Guidelines also recommend imaging if symptoms don’t resolve after 6 weeks of conservative treatment. Or if red flag symptoms occur, like progressive neurological deficits (8). Your physical therapist or primary care doctor will keep an eye out for red flags that could warrant imaging.
Learn more about red flag symptoms for low back pain at the end of this article.
So Why Does My Spine Hurt?
I endured chronic low back pain through high school and college. Was it a muscle? A disc? A bone spur?
X-Rays didn’t clarify the problem. Nobody seemed to know why my back hurt. It left me frustrated and exasperated, uncertain what to do next.
Eventually I learned how to treat it. You can read my story to learn what finally relieved my pain.
Testing and imaging don’t usually tell us the source of spine pain. It’s not as simple as taking an X-Ray and visualizing the problem.
Despite highly advanced imaging techniques, 85% of low back pain is considered nonspecific and an anatomical cause can’t be identified (9). Pain is complex, the aggregation of many factors.
Spinal pain is strongly influenced by activities, postures, stresses, beliefs, sleep, nutrition, and other factors. Especially for chronic pain issues, pain doesn’t equal damage.
The Good News
The poor relationship between imaging and spine pain should encourage you. You aren’t your X-Ray.
Here are 5 pieces of good news for spine pain.
1) Pain is Complex
Since pain stems from many factors, many treatments can relieve pain. Reducing stress, sleeping better, exercising regularly, adopting more positive beliefs, doing strengthening exercises–these are all routes to pain relief.
2) Positive Natural History
Acute neck and back pain typically resolve themselves, though intermittent flare ups are common.
3) Spines Get Stronger
The spine grows stronger in response to load, much like a muscle. Vertebrae (spine bones) get stronger with loading. This is known as Wolff’s law.
Discs also respond positively to loading. Runners have thicker discs than sedentary individuals (10).
4) Disc Injuries Heal
Research shows that disc herniations resolve on their own. While anatomical findings don’t always match up with pain, it’s reassuring to know that disc problems heal by themselves (2).
5) Pain Isn’t Damage
Pain, especially persistent pain, isn’t closely correlated to tissue damage. Spine pain rarely indicates damage and most acute discomfort subsides by itself.
Start Here
Physical therapy is a great option for back and neck pain. Active, exercise-based treatments work best for most cases of spine pain.
Passive treatments, like trigger point dry needling, spinal manipulation, and manual therapy can accelerate recovery when combined with an exercise-based approach.
Stay active and see a PT.
Doing physical therapy first leads to lower likelihood of opioid prescription and advanced imaging (11). And it’s more cost-effective than injections and surgery (12).
Physical therapists know when to refer patients to another doctor–when symptoms aren’t improving or if there are red flag signs. But as we discussed earlier, X-rays and MRIs are usually not recommended for neck and back pain. Unnecessary imaging can delay recovery.
Check out these articles for more spine pain insights:
15 Powerful Mid Back Pain Moves
Lower Back Pain and Can’t Straighten Up? Here’s Why
Readers: Have you ever gotten an X-Ray or MRI on your spine? What did it show? Did it help your recovery or make you afraid to move? Let me know in the comments.
For more practical rehab tips, join the free, fast-growing Facts & Physio Newsletter. Plus, get The Recovery Checklist when you sign up.

