Here are the tell-tale signs you might need plantar fasciitis rehab:
A Bad Start: Your feet hit the floor in the morning. And your leg almost collapses. It’s the searing heel pain again.
False Hope: Pain eases after a few steps. It’s less intense once you get your shoes on. And it eases throughout the day, but never truly goes away.
A Sad End: Plantar fasciitis pain often ramps up at the end of the day, especially if you walked or stood a lot. Then the cycle begins all over again the next morning.

Sound familiar?
This guide will tell you everything you need to know about plantar fasciitis rehab.
You’ll learn what causes plantar fasciitis, the top 3 risk factors and the 5 best plantar fasciitis rehab interventions for pain relief.
Let’s get started.
Who Gets Plantar Fasciitis?
Plantar fasciitis is a common foot problem. About 10% of people suffer from plantar fasciitis in their lifetime (1). It’s characterized by stabbing heel pain on the bottom of the foot.
Plantar fasciitis is most common for people ages 40-60, but it can torment individuals outside this age range (1). It’s also known as tennis heel, jogger’s heel, policeman’s heel, heel spurs and plantar fasciopathy (2).
A Nerdy Note
The term fasciitis implies inflammation (-itis = inflammation). But plantar fasciitis is not an inflammatory disease process, according to tissue research (3).
The term plantar fasciopathy is now the preferred medical term (-pathy = pathology) since it describes the disease process more accurately. However, since plantar fasciitis is the most well-known term, I will use it in this article.
What is the Plantar Fascia?
The plantar fascia attaches to the calcaneus, or heel bone, and extends to all 5 toes. It’s a thick piece of non-contractile connective tissue.

The plantar fascia is not a muscle. More like a thick piece of beef jerky. It is tough, dense and not easily stretched.
What Does the Plantar Fascia Do?
The plantar fascia’s main jobs are to maximize walking efficiency and support the arch of the foot. It performs these roles via the windlass mechanism.
Here’s how the windlass mechanism supports the arch and increases gait efficiency:
The plantar fascia is tensioned when the toes extend during push-off. Tension through the plantar fascia raises the arch of the foot, allowing the foot to act as a “rigid lever” for powerful propulsion (4).

The plantar fascia also generates elastic energy to improve gait efficiency.
During the push-off phase of gait, the toes extend, tensioning the plantar fascia, Achilles tendon and calf muscles. These structures then act as a spring, propelling the foot forward as it leaves the ground.
What Causes Plantar Fasciitis?
Plantar fasciitis is an overuse injury caused by overloading the plantar fascia.
Despite its name, there’s little inflammation with plantar fasciitis. At a tissue level, it’s a degenerative, non-inflammatory condition.
Subsequently, strategies to remodel the plantar fascia tissue work better than anti-inflammatory treatments.
Does Plantar Fasciitis Require Surgery?
Most plantar fasciitis cases do not require surgery. Plantar fasciitis responds well to conservative treatment.

It’s considered self-limiting, which means it usually resolves on its own. Unfortunately, pain resolution is slow without treatment.
With proper plantar fasciitis rehab, 80% of patients have significant improvements in 12 months (1). Surgery is rarely necessary. And it’s a last resort if conservative treatments fail (1).
Am I at High Risk for Plantar Fasciitis?
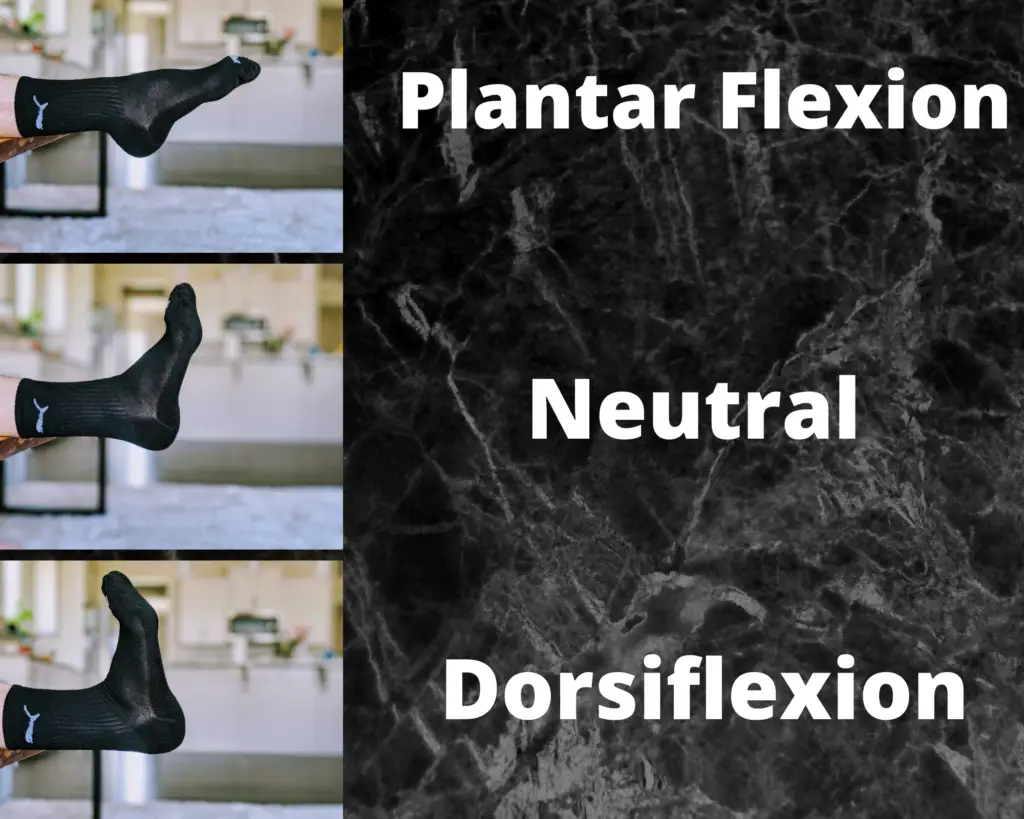
There are 3 strong risk factors for plantar fasciitis. Decreased ankle dorsiflexion range of motion, obesity, and increased time standing/walking at work are all significant risk factors (1).
People with 0 degrees or less of ankle dorsiflexion range of motion are 23 times more likely to have plantar fasciitis (5).
Having high arches or a low arches may increase the likelihood of plantar fasciitis, but arch height isn’t a strong risk factor.
What are Common Symptoms of Plantar Fasciitis?
Symptoms of plantar fasciitis worsen after prolonged rest periods (such as the first steps in the morning). Heel pain worsens when walking barefoot on hard floors and when wearing unsupportive shoes. Pain also increases after walking or standing for a few hours.
In my experience, the worst combination is carrying a golf bag for several hours, then sitting for a while. The first few steps are torturous!
Burning, numbness, tingling and weakness in the foot aren’t associated with plantar fasciitis. Likewise, swelling, warmth and a history of foot trauma are less indicative of plantar fasciitis.
If you have questions about your symptoms, consult with a qualified healthcare provider, like your local physician or physical therapist.
Plantar Fasciitis Rehab Options
There are dozens of plantar fasciitis rehab treatments. Some work wonders. And others are utterly useless. Buckle up, there are a lot to cover!
Let’s start with the simplest, least aggressive options before discussing the most invasive.
Taping
Plantar fasciitis taping is thought to reduce stress through the plantar fascia. Taping techniques pad the heel and support the arch of the foot (subsequently off-loading the plantar fascia).

Taping produces significant short-term pain relief (4,6). Low-dye taping is the most popular taping techinque for plantar fasciitis rehab.
Check out this video to learn it’s done:
Want to try it? Grab some tape here.
Taping won’t fix the underlying issue. And it’s probably not the “one weird trick” that solves your plantar fasciitis forever. But it can make day-to-day activities much less painful.
Shoe Orthotics
Shoes inserts are one of my favorite plantar fasciitis rehab treatments.

Orthotics are inexpensive, easy to implement, and supported by research (1). Shoe inserts support the arch and reduce loading through the plantar fascia. Walking feels better and the sun shines a little brighter.
Before you rush out to have a $400 custom orthotic molded to your foot, consider an off-the-shelf option. Studies find similar benefits between off-the-shelf and custom orthotics for plantar fasciitis (1).

However, custom orthotics may work best for unique foot shapes and unusually high or low arches.
A gel heel cup is another excellent option to dissipate force through the heel and take stress off the Achilles tendon and plantar fascia (4). Click the image to check out these heavy-duty heel cups:

Even a 3D-printed heel cup can alleviate heel pain! (7)
Footwear
Comfort is key.
Matching footwear to foot shape doesn’t consistently reduce injury (7,8). Your foot shape is different than mine. Shoes that are comfortable for you might not be comfortable for me. And vice versa.
So find shoes that feel good.
Another key footwear strategy for plantar fasciitis rehab: Wear different pairs of shoes throughout the week. Regularly rotating shoes helps those with physically demanding jobs.
Auto assembly plant workers who wore at least two pairs of shoes each week had 72% less plantar fasciitis than those who wore the same shoes every day (9).
Stretching
Stretching is the most common plantar fasciitis rehab technique – and for good reason! Calf muscle and plantar fascia stretching is a fantastic treatment for plantar fasciitis (1,3,4).
72% of study participants had less pain after an 8-week stretching program. Those who stretched and wore off-the-shelf orthotics get even better results! (10)
Here are 3 stretches for plantar fasciitis.
1) Weight-Bearing Gastrocnemius Stretch

Perform these with a straight knee to target the gastrocs, which cross the knee joint. Support the arch (as I’ve done here with a folded towel) to increase the stretch on the calf muscles (11).
2) Weight-Bearing Soleus Stretch

To target the soleus, which does not cross the knee, perform these with a bent knee. Keep the arch supported and toes forward. You should feel this stretch in your lower calf and Achilles tendon.
3) Great Toe Extension Stretch

This stretch targets the plantar fascia directly and addresses mobility deficits at the distal end of the plantar fascia.
Optimal stretching dosage is variable. It depends on irritability of symptoms. 3 sets of 30 seconds, twice a day is a conventional prescription.
Quiz
Q: What’s the biggest risk factor for plantar fasciitis?
A: Limited ankle dorsiflexion (see risk factors section above)
Why does stretching work? Stretching the calf muscles increases ankle dorsiflexion mobility.
Calf stretches reduce tension through the Achilles tendon and subsequently the plantar fascia (4). Stretching may also remodel degenerating tissue in the plantar fascia.
Strengthening
Beefing up the plantar flexors, primarily the gastrocnemius and soleus muscles, accelerates plantar fasciitis rehab and pain relief(1). One study found that calf strengthening was more effective than stretching over a 3-month span (12).
Here are 3 stellar options for strengthening the plantar flexors:
1) Double Leg Calf Raise
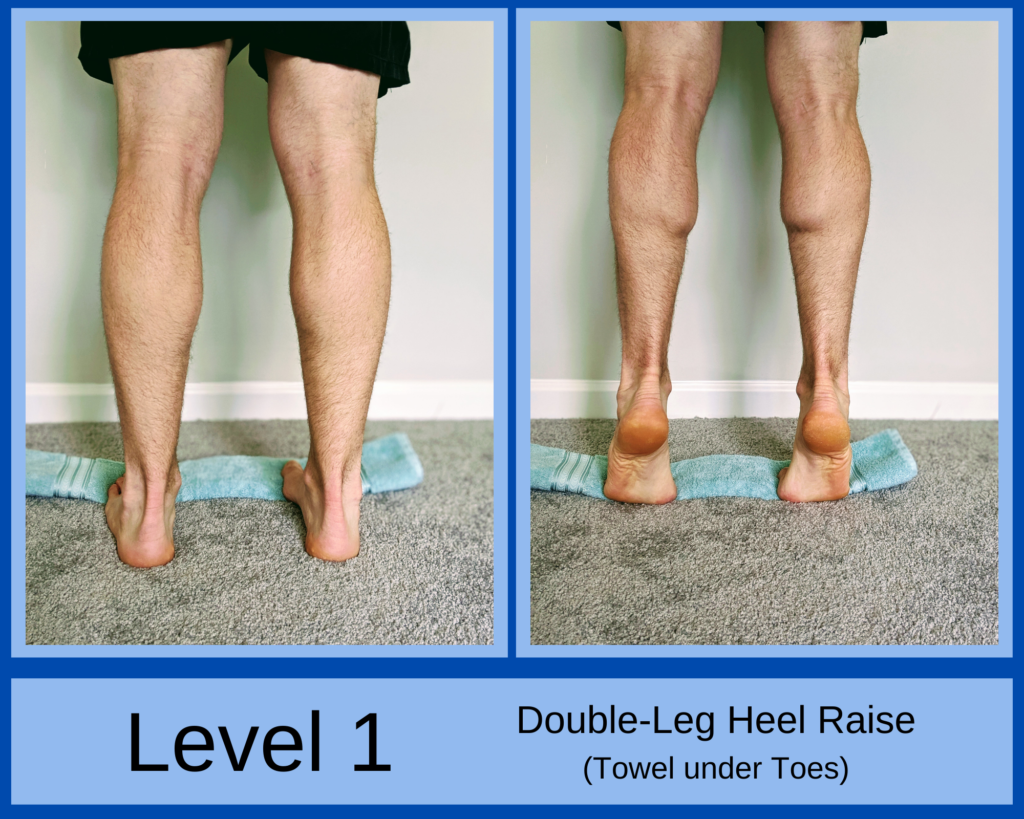
Raise and lower at a controlled pace using both legs. Place a folded towel under the toes to elongate the plantar fascia and increase stress through the tissue. The plantar fascia strengthening vs. stretching study (12) used the towel-under-the-toes technique with excellent results.
2) Double to Single Leg Calf Raise

Raise with both legs, shift your weight to the painful leg, then slowly lower with the painful leg. This exercise is an ideal stepping stone between double leg calf raises (Level 1) and single leg calf raises (Level 3).
3) Single Leg Calf Raise

Finally, the most challenging option is single leg heel raises. Perform slowly, through full range of motion for maximum benefit. If level 3 becomes too easy and you can crank out 20+ high-quality reps, hold a weight or wear a heavy backpack to make it tougher.
Strength exercises help remodel the plantar fascia and improve its tolerance to loading. These exercises may too uncomfortable when pain is extreme. But they’re effective if they’re tolerable.
Like stretching, dosage depends on irritability and pain levels. Pick one variation you can do without severe pain or difficulty.
2-3 sets of 8-15 repetitions is a reasonable starting point for most people. Performing calf raises 3-4 days/week is proven to relieve plantar fasciitis better than stretching (12).
Dry Needling
Trigger point dry needling involves inserting a thin, solid needle into a muscle at the location of a tender, palpable band.
Dry needling is not a do-it-yourself technique.
Please do not try this at home. Your tibial arteries will thank you.
Many physical therapists (myself included) perform dry needling, and other medical professionals use it too. Dry needling is a proven treatment to reduce heel pain (13).
Trigger points in the medial gastrocnemius and soleus can cause pain referral to the heel. Dry needling these tender areas can ease heel pain and speed up the plantar fasciitis rehab process.
To learn more, check out The Ultimate Guide to Dry Needling
Night Splints
Night splints are like eating kale. Unpleasant but effective. They’re easy to use. But not-so-easy to use consistently.
A night splint is worn while asleep (or tossing and turning). It keeps the ankle in a neutral position.
We often sleep with our toes pointed down, which puts the plantar fascia in a short position. Then we lengthen and load the plantar fascia once our feet hit the floor in the morning.
No wonder the first step feels like stomping a Lego!
Night splints reduce plantar fasciitis pain, but their bulkiness limits patient adherence (3). Instead of the full boot night splint, I prefer a less cumbersome dorsal splint:

Manual Therapy
Manual therapy is hands-on treatment by a professional.

Though not a great stand-alone treatment, manual therapy in addition to exercise is highly effective for plantar fasciitis rehab (14).
Manual therapy for plantar fasciitis relief involves mobilizing stiff joints and treating tight or restricted muscles. Assessing and treating the right joints and muscles is key.
Your local PT can help. Physical therapists study for 7 years to understand the intricacies of human anatomy and movement.
The research is in: plantar fasciitis rehab is suboptimal without manual therapy (14).
Soft Tissue Mobilization
These techniques mimic soft tissue treatment provided by a physical therapist. They decrease muscle tone and improve tissue mobility.
1) Plantar Fascia Self-Mobilization

Given the immense strength and density of the plantar fascia, this technique does not stretch the tissue (15). However, it can desensitize the area and improve tissue mobility around the plantar fascia.
Your force into the ball should be based on pain levels and irritability–uncontrollable sobbing and bleeding from the eyes are two signs you’re mobilizing too aggressively.
For me, this is a go-to pain relief exercise if my heel starts hurting.
2) Calf Self-Mobilization

Place a ball under the calf muscles. Find a sore spot and hold pressure on it. To intensify the exercise, use a firmer ball or pump your foot up and down as you hold pressure on the tender area.
A hard rubber ball, like a lacrosse ball, works best for calf self-mobilization. This technique treats myofascial trigger points in the gastrocnemius and soleus muscles which can refer pain into the heel.
Combining soft tissue treatment with stretching is more effective than stretching only (14).
3) Percussion Therapy
Massage guns are a hot trend in the fitness and rehab world right now. And for good reason!
I use percussion therapy in the PT clinic to reduce muscle tone and alleviate patients’ pain. It’s my patients’ favorite treatment.
For plantar fasciitis rehab, percussion therapy works best on the calf and lower leg muscles. Proceed with caution around bony areas in the foot and heel. Massaging the wrong spot can exacerbate heel pain.

There are many percussion therapy tools you can use. Here are 3 great options:
Theragun PRO
This is a top-of-the-line massage gun. It comes with 6 different attachments and a rotating arm for easy ergonomics. It feels amazing on sore, tight muscles. Plus, it’s a quiet model with preloaded routines.

It’s easy on the body, less so on the wallet. Check the price here.
Hypervolt Plus
I use the Hypervolt in the PT clinic. My patients love it. It has 3 speeds and 5 attachments. The battery last up to 3 hours between charges.

At half the price of the Theragun Pro, it’s a sturdy, high-value option. See it on Amazon here.
Renpho Massage Gun
This one is a budget-friendly option for giving your muscles some TLC. Plus, it’s rated 4.6 on Amazon (over 26,000 reviews) and comes with 5 attachments.

Extracorporeal Shockwave Therapy
ESWT sends shockwaves into the foot to treat plantar fasciitis. It’s proposed to have pain relieving effects. This treatment is used if other conservative measures fail.
Effectiveness studies on extracorporeal shockwave therapy have mixed results (1,14). The benefits don’t seem to outweigh the risks for this treatment. And higher quality studies don’t support its use (14). Side effects include bruising, increased pain, severe headaches and swelling (16).
Personally, I’d try the 9 strategies listed above before ESWT.
Ultrasound
Therapeutic ultrasound involves applying sound waves to the painful tissue. Research guidelines recommend against using ultrasound to treat plantar fasciitis (14).
It’s most powerful effect is placebo.
Electrical Stimulation
E-stim is in the same boat as ultrasound. No additional benefit when added to a comprehensive treatment program (14). It’s a poor treatment choice for plantar fasciitis rehab.

Electrical stimulation is unlikely to cause direct harm or severe side effects. But the opportunity cost is substantial with so many effective alternatives!
Nerve Ablation
Also known as radiofrequency ablation, this procedure involves cauterizing (burning) a nerve in the foot. Afterwards, an area of numbness is left (where the seared nerve previously provided sensation).
There’s limited research on this technique, but early studies indicate it reduces pain for 85-90% of patients (17).
Personally, I’d try almost everything else before opting for this treatment. But nerve ablation can alleviate pain and prevent surgery.
Corticosteroid Injection
Steroid injection for plantar fasciitis has clear pros and cons.
Pro: It’s effective for short-term pain relief (1).
Con: It increases the likelihood of plantar fascia rupture (not ideal!) and fat pad atrophy (thinning of the fat pad on the bottom of your heel) (1).
Questionable effectiveness and serious risks give steroid injections a thumbs-down from a top physical therapy journal (14).
Surgery
Surgery is a last resort for plantar fasciitis if conservative treatments have failed (1). (And no, rubbing ice on your foot for 5 minutes last week doesn’t count as “failing conservative treatment”!)
I’m not an orthopedic surgeon; plantar fascia surgical interventions aren’t my area of expertise. Here are a few findings I stumbled across in the literature:
- Pain relief is common after a plantar fascia release (1)
- Complications can include arch collapse, midfoot pain and heel pain (1,18)
- Gastrocnemius lengthening may be an effective alternative to plantar fascia surgery, with fewer complications (18)
Believe it or not, there are even more plantar fasciitis treatments we didn’t cover. I chose these 15 options because they’re either the best or the most popular.
My Top 5 Treatments
Personally, I have suffered from mild plantar fasciitis on a few occasions. If it flared up again, I would use these 5 rehab treatments:
- Adjust my footwear by finding ultra-comfortable shoes. I’d support my slightly-flat feet with an off-the-shelf orthotic. A heel cup is another solid option. I might even ask my younger brother to make one on his 3D printer.
- Rotate my shoes and wear two or three pairs to work throughout the week.
- Stretch my gastrocs, soleus and plantar fascia.
- Treat soft tissue impairments with self-mobilization strategies, dry needling and manual therapy.
- Strengthen my calf muscles to increase the loading tolerance of my plantar fascia.
Readers: What plantar fasciitis treatments have worked for you? Which ones haven’t? Share your experience in the comments.
For more proven pain relief insights, join the free, fast-growing Facts & Physio Newsletter. Plus, get The Recovery Checklist when you sign up.
References
- https://www.aafp.org
- https://emedicine.medscape.com
- https://www.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://pubmed.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://journals.sagepub.com
- https://bjsm.bmj.com
- https://deepblue.lib.umich.edu
- https://pubmed.ncbi.nlm.nih.gov
- https://pubmed.ncbi.nlm.nih.gov
- https://pubmed.ncbi.nlm.nih.gov
- https://www.ncbi.nlm.nih.gov
- https://www.jospt.org
- https://jaoa.org
- https://pubmed.ncbi.nlm.nih.gov
- https://www.podiatrytoday.com
- https://www.ncbi.nlm.nih.gov

