Frozen shoulder, also known as adhesive capsulitis, is a bizarre disease process. It causes moderate to extreme shoulder stiffness, pain and disability (1,2).
Frozen shoulder is like my motivation to eat vegetables; it appears without warning and disappears just as mysteriously. Except frozen shoulder lasts longer.
Here are the facts on frozen shoulder:
1) Frozen shoulder affects 2-5% of the U.S. population
It sounds like a small percentage, but frozen shoulder affects millions of people (3). For perspective, 4.8% of Americans are their parents’ only child. 3.9% of the U.S. population lives in Illinois. The odds of rolling snake eyes on two dice? 2.8%

2) Frozen shoulder is common from 40-60 years old
It’s a midlife crisis for your shoulder. Unfortunately, this disease afflicts people in their working years (1). It disrupts work, sleep, and playing catch with the kids.
3) Women have frozen shoulder 4x more than men
The reason for this difference is unclear (2). Men are notorious for delaying and avoiding medical treatment, and research supports this stereotype (4). Since they’re reluctant to seek treatment, men are diagnosed with frozen shoulder less often than women. Other unknown factors likely contribute to the diagnosis disparity between men and women.
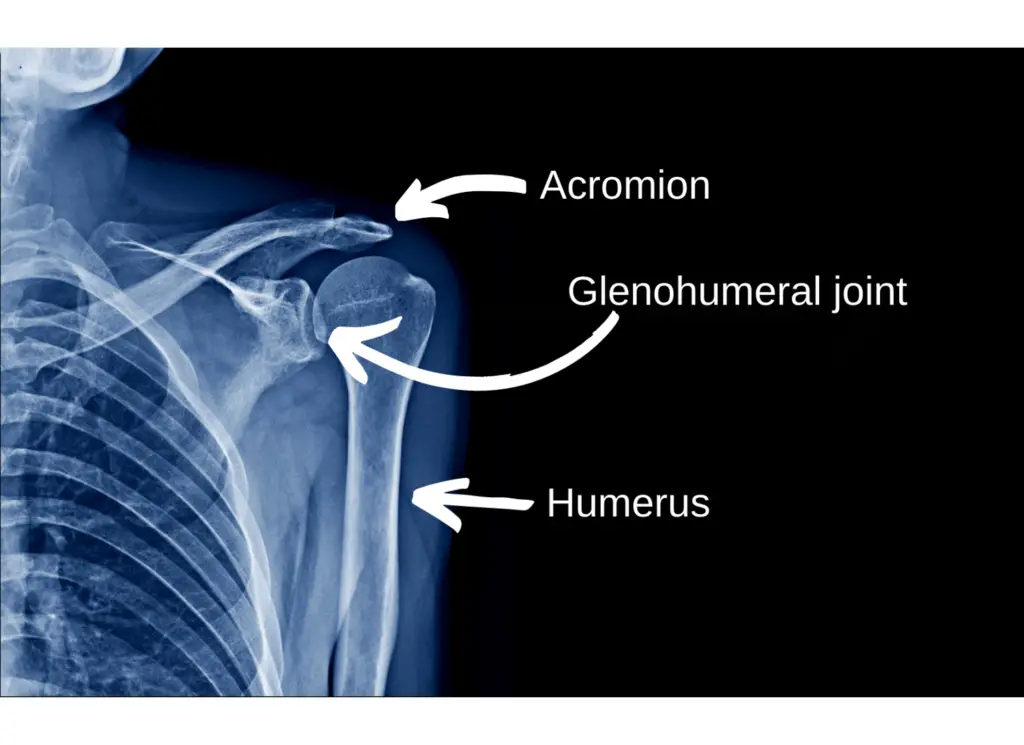
4) No tests diagnose frozen shoulder
Diagnosis is made from physical examination, medical history and imaging findings (well actually, lack of imaging findings). It’s a diagnosis of exclusion, meaning other pathologies are ruled out before the frozen shoulder diagnosis is finalized (2).
Risk factors (see #6) increase a clinician’s suspicion of frozen shoulder. X Rays and MRIs are unremarkable unless there’s an underlying rotator cuff injury.
In the physical examination, extreme stiffness into external rotation is evident.
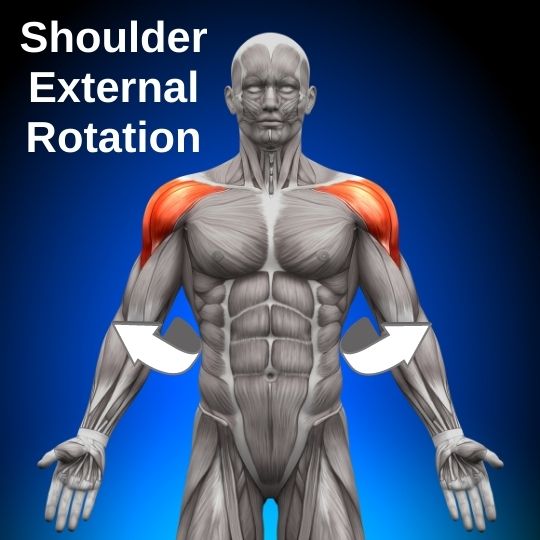
Limited shoulder external rotation is a key indicator of frozen shoulder. As they say: if it looks like a duck, sounds like a duck, and walks like a duck, it’s probably a frozen shoulder.
5) Most frozen shoulder cases are unexplained
These inexplicable cases are called “primary frozen shoulder.” Primary frozen shoulder begins without injury, surgery, or shoulder trauma.
6) Some cases have a clear cause
Common causes of “secondary frozen shoulder” include trauma, rotator cuff pathology, stroke, heart disease, and diabetes (1). Other risk factors include thyroid disorders, cancer, and Parkinson’s disease (2).
If risk factors were football players, diabetes would be Tom Brady. It’s in a league of its own. Frozen shoulder afflicts a whopping 20% of diabetics! (2)
7) Frozen shoulder involves inflammation
The disease process is controversial, but tissue studies indicate inflammation plays a key role. Inflammation of the ligaments, joint capsule, and connective tissue around the shoulder joint causes pain and restricts motion. The term “adhesive capsulitis,” another name for frozen shoulder, refers to adhesions and joint capsule swelling at the glenohumeral shoulder joint.
Want to learn more about the tissue changes? Check the references (2) to learn about cytokine-mediated synovial inflammation, B-lymphocytes, and fibroblastic proliferation (oh my!).
8) Frozen shoulder lasts 2.5 years
Its duration ranges from a few months to a few years, with an average length of 30 months (2).
It’s stubborn, like a house guest who’s worn out his welcome. You can try gentle coaxing or aggressive manipulation, but it goes away at its own pace.
You have to win the waiting game, and you’ll be waiting longer than you want. Fortunately, several treatments make the waiting more bearable and accelerate the recovery process. See #12 and #13 for more.
9) Frozen shoulder has 4 stages
Stage 1: Prefreezing
Symptoms include shoulder pain and mild stiffness, particularly with external rotation. Frozen shoulder is rarely diagnosed in stage 1. At this stage, it presents like shoulder impingement or osteoarthritis. This stage lasts 1-3 months (3).
Stage 2: Freezing
Shoulder motion progressively worsens. Pain worsens too, often disrupting sleep. Diagnosis is possible during stage 2. At this stage, pain and stiffness limit shoulder function (3).
Stage 3: Frozen
Not nearly as fun as the movie, this stage is characterized by extreme stiffness. Pain levels are high at first, but decrease gradually during this stage (3).
Stage 4: Thawing
After a year or more of shoulder pain, symptoms finally improve. Stiffness begins to ease, and pain levels plummet (3). The grass looks greener, the birds sing sweeter, your teenage kids aren’t so insufferable. It’s a new day.
10) Frozen shoulder gets better by itself
Regardless of treatment, the shoulder hurts less and loosens up on its own. Stiffness can persist, but most people have a satisfactory outcome (2).
11) 10% have residual pain or stiffness
Diabetics tend to have worse outcomes, but most cases fully resolve with time (2). Lots of time.
12) Physical therapy helps
PT treatment, including range of motion exercises and joint mobilizations, reduces shoulder stiffness (1,2,3,5). Gentle to moderate intensity shoulder mobility exercises can limit the loss of shoulder motion through the 4 stages of frozen shoulder (2).
13) Steroid injections reduce pain
Corticosteroid injection into the shoulder joint is arguably the best treatment for frozen shoulder. It won’t help you hit home runs (that’s anabolic steroids) but it provides powerful pain relief that lasts up to 6 months (5).
14) The non-dominant arm usually freezes
Fortunately, the dominant arm isn’t affected as frequently (2). Don’t ask me why. I don’t know. But it’s a rare piece of good news for frozen shoulder.
15) The other shoulder can freeze
Within 5 years of the first frozen shoulder, the opposite shoulder freezes 15% of the time (2). It’s not a foregone conclusion, but having one frozen shoulder increases your risk of the opposite shoulder freezing.
Final Thoughts
Frozen shoulder is unpleasant. And it takes a while to resolve.
But on the bright side, frozen shoulder is self-limiting and heals on its own. Treatment options like physical therapy and cortisone injection help, too. And 90% of cases resolve without permanent deficits.
In my experience, frozen shoulder is occasionally over-diagnosed. In some cases, chin tucks (treatment #1 here) immediately improve shoulder pain and motion. Also, dry needling can rapidly resolve shoulder pain that isn’t from a true frozen shoulder.
If you have a frozen shoulder, consider working with a skilled physical therapist and an orthopedic or sports medicine physician to develop the best treatment plan for you.
Is pain waking you up at night? Check out these strategies to ease shoulder pain during sleep.
For more evidence-based insights you won’t find anywhere else, join the free Facts & Physio Newsletter. Plus, get The Recovery Checklist when you sign up.

